Neonatal and childhood dysphagia: keys to detecting and treating swallowing difficulties
Swallowing is defined as the activity of transporting solid and liquid substances and spit from the mouth to the stomach. This mechanism is achieved thanks to forces, movements and pressures within the oropharyngolaryngeal complex (Rodriguez Mendez, et. al., 2021). In other words, the ability to hold food in the mouth, chew it if necessary and prepare the food bolus inside the mouth to subsequently swallow it and transport it through the larynx, passing through the esophagus to the stomach.

What do we mean by dysphagia?
The European Society for Swallowing Disorders (ESSD) defines dysphagia as the medical term used to represent ‘swallowing difficulties’. They explain that people with dysphagia may have problems consuming certain foods or liquids and others may not be able to swallow at all. These people may have problems sucking, swallowing, drinking, chewing, eating, swallowing saliva, closing their lips to control the contents of their mouth, or they may often experience that solid or liquid foods do not follow the correct path to the stomach. It should be noted that dysphagia can affect anyone regardless of age or lifestyle. There are causes such as accidents, trauma, cancer and its treatment, respiratory or degenerative conditions, which increase the likelihood of suffering dysphagia. Similarly, it can appear in children with difficulties from birth (ESSD, 2024).
Neonatal dysphagia is defined as dysphagia affecting children between 0 and 6 months of age, and infantile or paediatric dysphagia is defined as dysphagia between 6 months and 24 months, the age at which a complete chewing pattern is achieved. Difficulties differ in terms of developmental stage, given that from 0 to 6 months it will affect the swallowing-suction-breathing pattern and infantile dysphagia will involve alterations in learning to chew, the creation of the food bolus, tongue propulsion and swallowing, taking into account the changes in textures and volumes at each stage of development (Matarazzo, 2024).
These difficulties may be based on neurological alterations, physical alterations, prematurity, among others. Depending on the causes and the time of onset, we will observe one or other difficulties and the repercussions on the health of children will be of different magnitude.
Swallowing in the first stages of life.
The full-term baby without cognitive or physical alterations.
Babies are born to feed, sleep and interact with their mother. They are born with in utero learned oromotor skills (lip, intraoral and lingual movements for sucking and swallowing) as well as the innate seeking and opening reflexes (Matarazzo, 2024). At birth, the infant seeks contact with the mother and initiates the search reflex to initiate feeding. It climbs to the breast and initiates stimulation of the breast and triggers the sucking-sucking-swallowing-sucking pattern. This same pattern appears in formula-fed infants. The following table shows the oral position of the baby (bottle and breast) and each moment of the swallowing pattern:
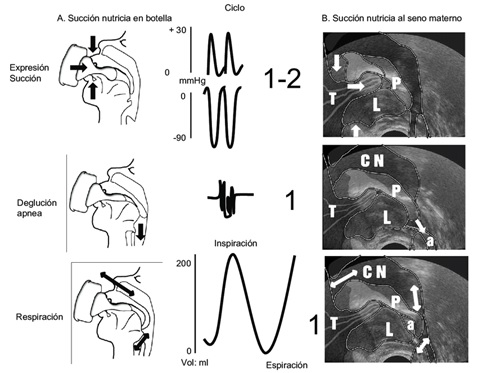
As can be seen, the baby has control of its nasal breathing, as well as the management of the liquid inside the oral cavity. In the same way, it has the ability to control the movements and the force to be exerted at any given moment, whether of the lips, gums, cheeks or tongue.
Neonatal and infantile dysphagia. Concept, causes and treatment.
Babies and infants with alterations in the swallowing process.
If there is any prenatal, perinatal or postnatal alteration that puts any of these oromotor or reflex skills at risk, it will lead to an alteration in oral swallowing. Whether due to lack of development of the central nervous system (CNS), lack of development of the organs involved in swallowing, physical alterations or several at the same time, these babies have an atypical swallowing development. The most common cases are premature and very premature babies, babies with oral morphological alterations (lip or palatal clefts), babies with other conditions involving malformations or motor difficulties, situations that occur in the infant population.
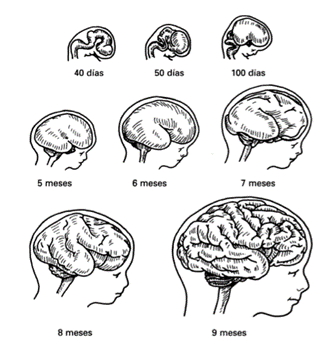
Most of these babies, for medical reasons, are taken to NICUs (neonatal intensive care units) where they are sometimes separated from their mothers, so they are forced to develop and learn in a decentralised way: outside the womb, without their mother nearby, in a hostile environment (lights, tubes, lines, sounds...). It must be understood that oral feeding skills in the healthy preterm baby depend on the maturation of the central nervous system (Matarazzo, 2024). As can be seen in the following image, it is in the last stages of uterine gestation that the brain undergoes significant morphological developmental changes.
Depending on the moment of birth and the associated medical needs, we will have babies with no alterations, or babies with difficulties in activating reflexes, with difficulties in grasping the teat, with difficulties in carrying out the correct tongue movement, with difficulties in carrying out suction-swallowing-breathing coordination, with difficulties in carrying out swallowing apnoea... All actions necessary for swallowing to be effective and not entail a risk to their development and well-being.
If we look at the degree of swallowing inefficiency they present, and the degree to which their vital security is affected, these babies are fed through nasogastric tubes (NGT) until oral swallowing can be rehabilitated. If this is not possible or more rehabilitation time is required and the NG tube is used for more than 6 months, a PEG (percutaneous endoscopic gastrostomy) is usually inserted. These alternatives to the oral route allow us to ensure the nutrition, hydration and medication of these infants.
Assessment, treatment and evolution.
Logopaedic treatment aimed at correcting these alterations begins in the NICU, with family follow-up, teaching families how to feed their infants, carrying out the necessary treatments and adaptations to make swallowing effective, facilitating and ensuring the safety of each intake. After the period in the NICU, many of these babies continue to present difficulties and families need continuous support to feel secure at each stage of their baby's or infant's development.
Outpatient speech therapy allows families to be informed and accompanied throughout the process of their child's swallowing development and to deal with the different changes, adaptations and facilitations that appear over time: changes in their children's feeding methods, myofunctional treatment to ensure the correct pattern of movement and tone of the muscular structures involved in swallowing, advice on the introduction of different textures and new foods, monitoring to ensure the correct safety of ingestions, reassessments to monitor progress in each of the stages of development and coordination with the healthcare team that will monitor these infants.
Warning signs for consultation in the speech therapy service
Even if no difficulties have been diagnosed previously, if you see that your baby or child has difficulty breathing while eating, has difficulty gaining weight, cries or has watery eyes at feeding time, gets tired or even falls asleep at feedings, pulls away from the breast/bottle or fights with the teat, loses a lot of food from the corner of the mouth and/or opens his/her arms, do not hesitate to consult.